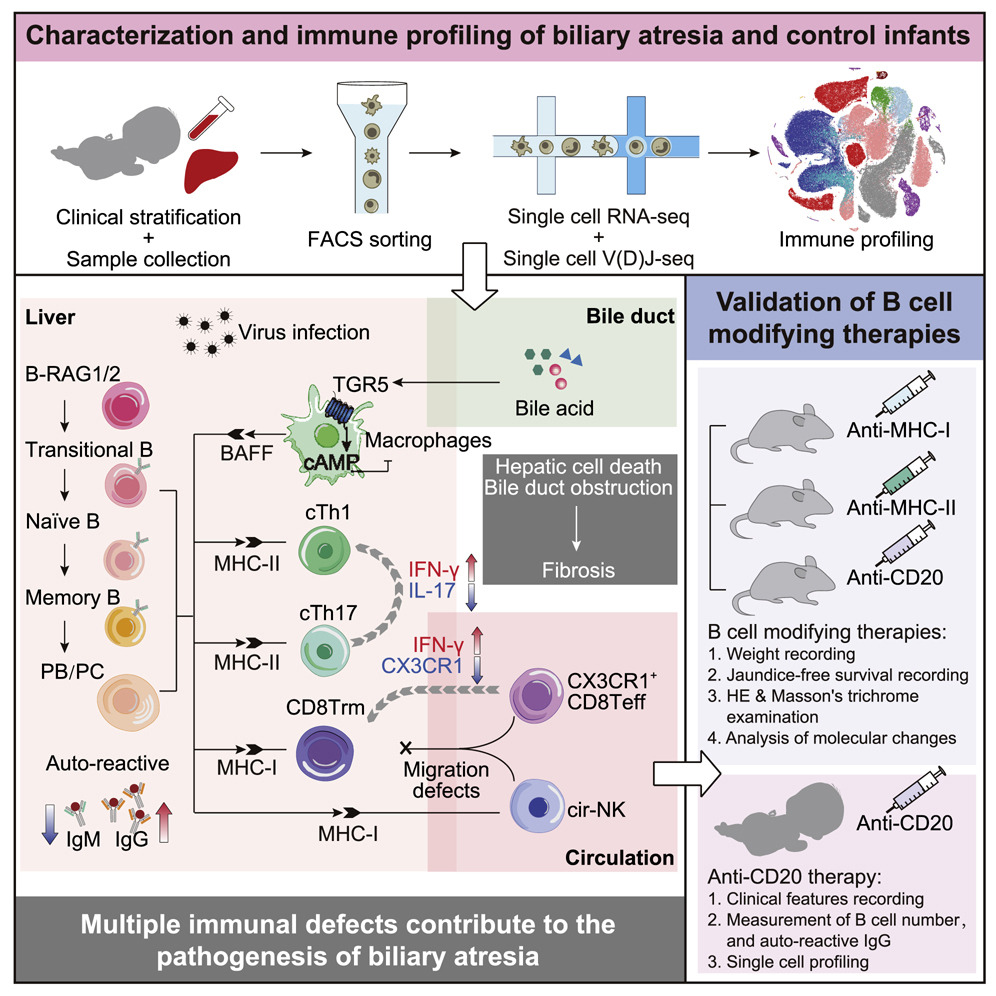
Dr. Yuxia Zhang's team provides comprehensive liver immune profiling in infants with biliary atresia and proposes B-cell-modifying therapies to alleviate liver pathology
An important function of the fetal liver is hematopoiesis (generation of red cells and immune cells), which peaks around 7-17 post conception weeks (PCWs). After 20 PCWs, bone marrow takes over the majority of the hematopoiesis function. In bone marrow, progenitor B cells undergo processes that eliminate B cell receptors that have high affinity to body's self-molecules. Defects in establishing B cell tolerance can cause autoimmune diseases that target and destroy body's self-tissues.
Perinatal infection has been associated with the development of biliary atresia (BA), an autoimmune liver disease that can cause rapid liver failure in infants. The pathogenic mechanisms occurring locally in the liver of infants with BA was incompletely understood. Dr. Yuxia Zhang's group from Guangzhou Women and Children's Medical Center, Guangzhou Medical University discovered that B cell lymphopoiesis in the liver was extended beyond birth, persisting through at least the first 3-4 months of life. They hypothesized that encountering of pathogens or self-antigens may expand the autoreactive B cell repertoire and promote development of BA. Indeed, IgG-specific autoantibodies were significantly increased in the liver of infants with BA.
Apart from producing autoantibodies, B cells may also modify the functions of T, NK, and myeloid cells through MHC-mediated antigen presentation and soluble mediators. In an RRV-induced BA mouse model, depletion of B cells by an anti-CD20 antibody, or blocking MHC-class-II- or MHC-class-I-mediated antigen presentation, significantly improved weight gain and decreased jaundice occurrence compared with untreated RRV mice. Unexpectedly, the scavenger function of Kupffer cells were also enhanced after treatment. In summary, B cell modifying therapies alleviated liver pathology in RRV-induced BA mouse model.
Based on the aforementioned findings, Dr. Zhe Wen and his clinical team performed a safety and efficacy study of rituximab (RTX) in an open-label pilot clinical study. A single dose of RTX was able to temporally deplete the mature B cells from the circulation and liver of infants with BA. They found that the beneficial effects were likely manifold, including halting the increase of IgG autoantibodies and preventing the expansion of cytotoxic T cells. Additional unexpected advantageous outcomes include increasing the inflammatory potential of macrophages, promoting the repairing function of CX3CR1+CD8Teff and cir-NK cells, and restoring the scavenger and regenerative function of Kupffer cells.
On November 27th, the article Liver immune profiling reveals pathogenesis and therapeutics for biliary atresia was published in Cell Journal. They provide a comprehensive description of immune dysfunction that leads to rapid liver failure in infants with BA and provide preclinical and clinical evidence showing that B-cell-modifying therapies may be used to restore liver immune function for infants with BA.
Dr. Yuxia Zhang, Dr. Zhe Wen, Dr. Huimin Xia from Guangzhou Women and Children's Medical Center and Dr. Fan Bai from Biomedical Pioneering Innovation Center (BIOPIC) are co-responders. Dr. Jun Wang, Dr. Yanhui Xu, Dr. Zhanghua Chen, Dr. Jiankun Liang, Dr. Zefeng Lin and Dr. Huiying Laing are co-first authors.
Yuxia Zhang
06 July 2021